Home » Campaign Country » BreastCheck: Saving lives and advancing breast cancer screening in Ireland for 25 years
BreastCheck
Saving lives and advancing breast cancer screening in Ireland for 25 years

Launched in February 2000, BreastCheck is Ireland’s free national breast screening programme and is part of the HSE’s National Screening Service. The programme was set up to reduce the number of deaths from breast cancer in Ireland.

At that time, the number of deaths from breast cancer among women in Ireland was one of the highest in the EU. This made the establishment of the breast screening programme a crucial response to this public health challenge.
We started by inviting women aged 50 to 64 for free breast screening. In 2015, we extended the eligible age range to include women aged 65, and by 2021 we were including all women aged 65 to 69. This change reflected emerging evidence that screening benefits women in this age range.
Programme delivery
BreastCheck is delivered within the framework of a BreastCheck Charter, which we updated in line with public feedback and plain language principles in 2025.
We invite women aged 50 to 69 for a free mammogram every two years. Most women are added to our BreastCheck register automatically. We get this information from the Department of Social Protection. Women can check the register online and if they are not on it, they can give us their details.
We offer a complete onward service to women who need it. This includes diagnosis, treatment and surgery.
We have a national network of mobile and static BreastCheck screening units. There are 4 static units in the East, South and West of Ireland. These units operate in tandem with mobile screening units where most women have their mammogram. 24 mobile units operate across 54 locations in Ireland, ensuring women can access screening close to where they live.

Programme uptake
We invite over 150,000 women for breast screening every year. Our most recent (provisional) data for 2024 shows the uptake rate at 72%, above our standard of 70% and among the highest in the EU.
- Uptake is highest among women who have attended for breast screening previously and are subsequently re-invited for screening in two years (85.6% in 2022, our latest published report).
- Among women invited for the first time, uptake is highest in women aged 50 to 54 (72.6% in 2022).
A quality-assured programme
From the outset, commitment to quality assurance and continuous improvement has been at the heart of BreastCheck. Our programme standards are based on the European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis, and in recent years we have contributed to the ongoing development and improvement of these guidelines.
BreastCheck has been accredited three times by the European Reference Organisation for Quality Assured Breast Screening and Diagnostic Services (EUREF), achieving our most recent re-certification in April 2025. This provides us with independent external reassurance of the high quality of our programme.
Workforce challenges
The early years of BreastCheck were marked by a shortage of radiographers, and this challenge has persisted, with global shortages of radiologists and radiographers posing ongoing difficulties.
The number of women eligible for breast screening in Ireland has grown quickly from 524,000 in 2019 to 625,000 in 2025. This increase is challenging because our clinical staff numbers have not grown at the same rate.
In a new development for the mammography workforce in Ireland, we have partnered with University College Cork to design and deliver a new postgraduate course in mammography. This flexible part-time course, which had its first student intake in September 2025, is the only mammography course available in Ireland. The course is for qualified radiographers and is delivered online, making it accessible to international students and extending its impact beyond Ireland.
Embracing advancements in technology
BreastCheck has consistently embraced technological advancements to improve the screening process. In 2008, we became the world’s first national breast screening service to fully adopt digital mammography, which offered improved image quality and consistency compared to traditional film-based imaging. This milestone significantly improved diagnostic accuracy.
We have started exploring the potential of artificial intelligence in breast cancer screening, hosting a workshop in 2024 to examine its benefits and challenges. We’re now implementing an AI programme in the National Screening Service, developing a comprehensive 4-year AI implementation strategy (2026-2029). BreastCheck will be the first national screening programme to explore the use of AI, with recent international research providing compelling evidence of its potential in mammography.
Supporting women to choose screening
We prioritise clear, evidence-based, person-centred communications to support eligible women to make an informed choice about taking part in breast screening. Our communications have evolved based on research and feedback including surveys, focus groups and market research – providing insights into the barriers and motivators to screening.
We design and run large-scale, evidence-based campaigns to raise awareness of breast screening. Using digital, social, print, radio and outdoor advertising, we help people understand what screening is, what it can and can’t do, and how to take part. We work to make sure people can find information easily online when they search for breast screening.
We work to increase health literacy in screening and address the barriers to screening to improve equity. We have:
- developed accessible information including easy-to-read and plain English resources, and visual stories using photos and videos
- translated videos in 25 different languages
- produced a video with Irish Sign Language.
In 2025 we started providing BreastCheck appointment information on the HSE Health App. This is part of our continued work to strengthen our communications with our screening participants. We’ll be adding more BreastCheck features to the App over time, giving women simple, accessible ways to stay informed and in control of their breast screening journey.

Continuous improvement
In 2024 we introduced a modernised patient database system. Aligned with the HSE’s Digital Health Strategy, this new system aims to simplify and streamline workflows, allowing our BreastCheck team to focus more on direct patient care. We can access real-time data to track each screening participant’s journey and address any gaps in service delivery.
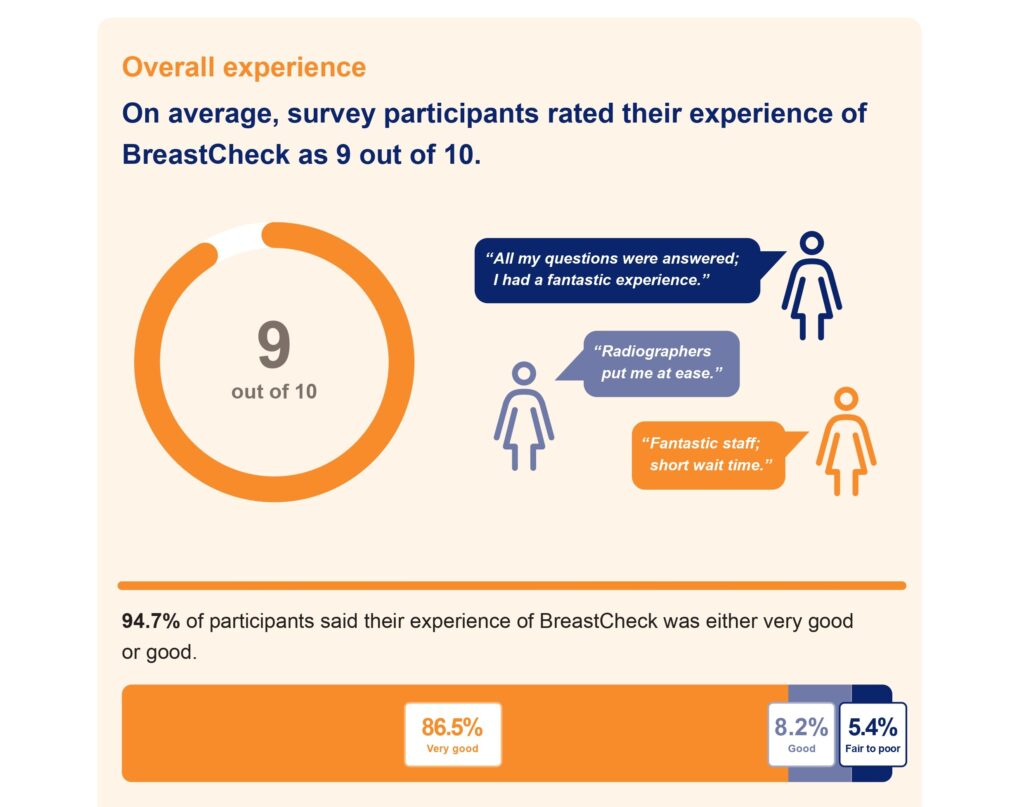
Our Patient Reported Experience Measures (PREMs) digital survey captures the experiences of women who take part in BreastCheck. This helps us to find out what we are doing well and where we can make improvements to our programme.
The impact of BreastCheck
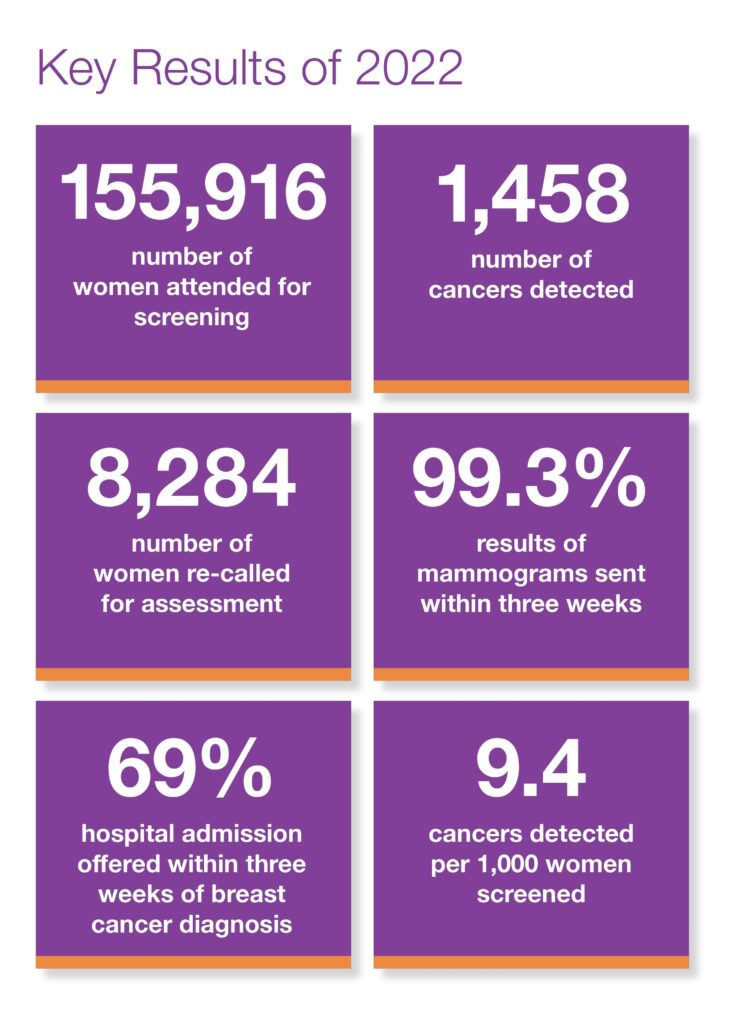
In its 25 years of operation, BreastCheck has performed over 2.6 million mammograms and detected over 18,000 cancers. Around one-third of all breast cancer cases diagnosed every year in Ireland are identified through the programme. Our breast cancer detection rate is one of the highest in Europe.
A 2022 report published by the National Cancer Registry Ireland shows that BreastCheck has significantly contributed to early-stage cancer diagnoses and reduced cancer-related deaths among women in the screening age range. These achievements underscore the programme’s life-saving impact and its vital role in Ireland’s healthcare system.